Abstract
Pregnancy and childbirth in women with myeloproliferative neoplasms (MPN) are subjects of increasing interest. MPNs are most commonly diagnosed in elderly individuals, however 10-20% of patients with MPN are of fertile age at diagnosis. Elevated risks of obstetric complications are described in MPN; miscarriage, stillbirth, preterm birth, and reduced live birth rates. Population-based data are limited, and data on fertility and reproductive patterns are lacking. We have previously performed a population-based study, including all pregnancies 1973-2017 from week 22 (week 28 before 2008) in patients with MPN in Sweden, comparing pregnancy outcomes to those of matched population controls. In 342 identified pregnancies in women with MPN we could confirm an increased risk of preterm birth in MPN compared to controls (12% vs 4%), while the rate of thrombosis (1%) and stillbirth (0.6%) was lower than previously anticipated in the MPN cohort.
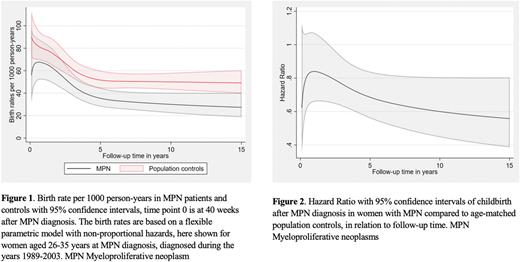
To further explore the childbearing potential of women with MPN we performed a study where women with a diagnosis of an MPN 1973-2018, aged 15-44 at diagnosis, were matched by age and year of birth to four population controls, free of MPN. Matching date was at MPN diagnosis, and follow up started 40 weeks after MPN diagnosis/matching date, thus excluding patients and controls that were pregnant at diagnosis. Patients and controls were followed until childbirth or censored at death, emigration, diagnosis of other hematologic malignancy, when turning 45 years old, or at the end of study, December 31st 2018, whichever occurred first. National health registers were used; Swedish Cancer Register and Patient Register to identify MPN patients, Register of Total population for identification of controls and migration data, and Multi-Generation Register to identify live births. Stillbirths were collected from the Medical Birth Register and miscarriages were collected from the Patient register. A flexible parametric model was applied, adjusting for matching variables, calendar period (1973-1988, 1989-2003 and 2004-2018) and age category at diagnosis (15-25, 26-35 and 36-44 years). Primary outcome was live childbirth after MPN diagnosis.
We identified 1,141 women with MPN and 4,564 controls with a mean age of 34 years at MPN diagnosis. Exclusion prior to start of follow up occurred in 730 women leaving 4,975 women left for analysis, 953 with MPN and 4,022 controls. Cause of exclusion was childbirth within 40 weeks of MPN diagnosis in 61 women with MPN and 189 controls. Regarding type of MPN, 24% were polycythemia vera patients, 54% essential thrombocythemia, 11% primary myelofibrosis and 12% MPN unclassifiable. Patients and controls were followed for 0-27.3 years, together collecting 25,532 person-years, and gave birth to 1,116 children. At MPN diagnosis mean number of previous live childbirths was 1.3 in women with MPN and 1.4 in controls, 61% of the women with MPN were parous at diagnosis and 67% of controls. Among those diagnosed 1989 and later, during the last 2 years prior to diagnosis, 2.5% of MPN patients and 1.9% of controls experienced at least one miscarriage.
Compared to childbirth patterns in controls, MPN patients had 28% lower rate of giving birth to a living child, hazard ratio was 0.72 with 95% confidence interval of 0.61-0.85, using a proportional hazards model. Birth rate per 1000 person-years was estimated using a non-proportional model, Figure 1. The HR of childbirth after MPN diagnosis in relation to follow-up time is shown in Figure 2. Of the women reaching age 45 during the study period, 17% of the MPN patients never had a child (before or after MPN diagnosis), the corresponding number in controls was 13%. The mean total number of children per women of those reaching age 45 during the study period, was 1.8 in the MPN cohort and 2.0 in population controls. There were one stillbirth in the MPN patients and 6 in the controls during follow-up.
This large population-based cohort study demonstrates a significantly lower hazard ratio of live childbirth in women with MPN compared to population controls. Reasons for this may be related to reduced possibility of having children, where difficulties conceiving, maintaining pregnancy, and obstetric complications may play a role, as well as related to the complex and highly personal decision to have children, affected by desire to have a child, life situation, health concerns, and expectations.
Disclosures
Björkholm:Takeda: Research Funding; Mundipharma: Other: Member of independent data monitoring committee; Incyte: Other: Member of grant committee; Astra-Zeneca: Honoraria; Roche: Honoraria; Pfizer: Honoraria; Bristol-Myers Squibb: Honoraria. Hultcrantz:Bristol-Myers Squibb: Membership on an entity's Board of Directors or advisory committees; Amgen, Daichii Sankyo, Cosette, GSK: Research Funding; Intellisphere LLC: Consultancy; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Curio Science LLC: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal